Researchers at the Skolkovo Institute of Science and Technology in Russia have devised a robotic limb that may help patients recover normal leg movement after suffering from spinal injuries or stroke. The robotic limb uses a brain-machine interface and electrical stimulation of the spine in order to help patients move their leg and help brain cells reestablish electrical communication with muscle cells responsible for regular movement.
One of the primary difficulties for those who have experienced traumatic spinal injuries or strokes is that both can result in a significant loss of movement. Both spinal injuries and strokes can weaken the electrical connections between brain cells and muscle cells, resulting in sporadic and decreased mobility. Oftentimes, patients who experience these injuries and suffer from weakened connections between their brain cells and muscle cells must undergo intensive physical therapy programs. While physical rehabilitation is beneficial for restoring these connections, it takes a significant amount of time and effort and can be a frustrating process for patients.
Now, Ivan et al. have designed a robotic limb that combines a brain-machine interface, electrical stimulation of the spinal cord, and virtual reality simulations to help patients recover their motor ability without undergoing the difficulties of traditional physical rehabilitation.
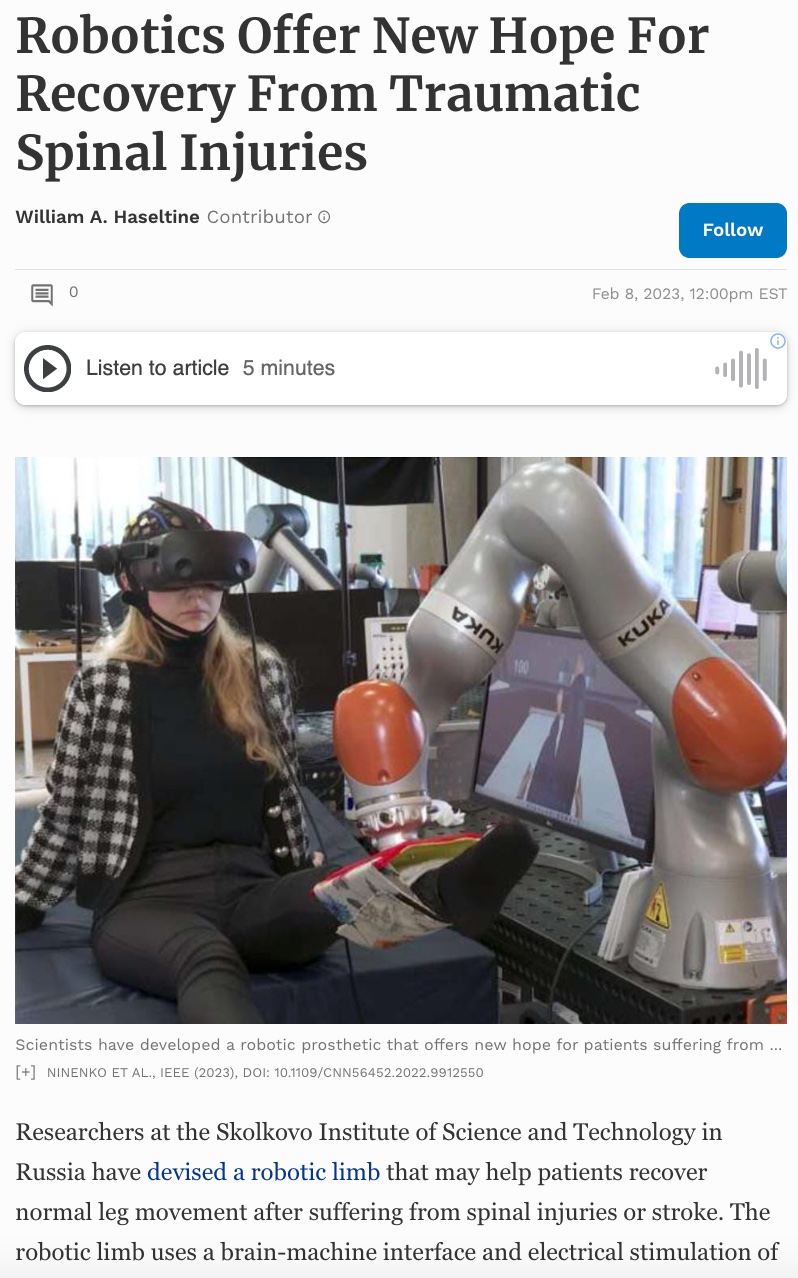
The robotic limb design was simple. Patients would sit on a chair and wear a virtual reality headset and non-invasive electrode cap. With the virtual reality headset, patients would see a scenario where there were six different tiles in front of them. When the patient thought about stepping onto a specific tile in the virtual reality simulation, the non-invasive electrode cap could detect electrical signals from the brain and transmit the signals to a computer. The computer could then interpret the brain signals and register the patient’s intention to move their leg. This would allow the computer to communicate that information to a robotic arm controlling the patient’s leg.

Figure 1: Patients wear a non-invasive electrode cap that can detect their brain signals.
NINENKO ET AL., IEEE (2023), DOI: 10.1109/CNN56452.2022.9912550
In the virtual reality simulation, the patient would see themself stepping onto the intended tile. At the same time, the robotic arm would move the patient’s leg for them in a way that mimicked the action of taking a step. As the robotic arm moved the patient’s leg, the patient’s spinal cord would simultaneously be electrically stimulated by non-invasive electrodes attached to the patient’s back.

Figure 2: In the virtual reality simulation, patients are tasked with visualizing themselves stepping onto different colorful tiles. A computer then decodes their brain signals and communicates the movement to a robotic arm that moves the patient’s l
NINENKO ET AL., IEEE (2023), DOI: 10.1109/CNN56452.2022.9912550
One of the important features of the robotic arm system is that Ivan et al. equipped the robot with highly accurate sensors. This allowed the robot to be capable of moving the patient’s leg in the precise way that the patient intended within the virtual reality simulation. The software controlling the robotic arm was also written so that the robot could mimic the natural trajectory of leg movements.
The theory behind this system was that by incorporating the virtual reality simulation and robotic arm, the researchers could effectively trick the brain into thinking that it was moving the patient’s leg as it normally would in a healthy person. By repeating the simulation over and over again, Ivan et al. theorized that they could trick the brain enough to eventually strengthen and rehabilitate the communication between the brain and the muscles.
This leaves the question of why Ivan et al. also incorporated electrical stimulation of the spinal cord. The researchers’ theory was that patients who have suffered from spinal cord injuries and whose connections between the brain and the muscles are weakened may still be sending electrical signals from the brain to the muscles. However, these signals may simply be weakened and not reach the threshold of voltage required to actually activate the neurons in the spinal cord. By incorporating spinal cord stimulations, Ivan et al. hoped to boost the electrical signals that the patients’ brains were already sending. This could help the patients rehabilitate the electrical connections through the brain and spinal cord until those neurons could function without any artificial support.
While the system was presented at the International Conference for Neurotechnology and Neurointerfaces, it has yet to be tested in a clinical setting. Ivan et al. hope that once they improve the system and can apply it to a clinical setting, the connections between the brain and the muscle in stroke and spinal injury victims will be rebuilt without the patient having to go through the frustrations of traditional physical therapy.
Overall, this system demonstrates real progress in the use of robots and brain-machine interfaces for clinical applications. However, it is important to keep in mind that while the system is innovative and an interesting approach to physical rehabilitation, it still has a long way to go before it can be applied in a clinical setting. It will be interesting to see how this project continues to evolve and whether it is actually effective in real patients.